Mobilization Orthoses to Increase Joint Range of Motion
Mobilization orthoses are an excellent tool to help patients regain passive joint motion. They are often used to treat patients with very stiff joints following injury or prolonged immobilization.
As a therapist, you can choose between the following types of mobilization orthoses:
- Dynamic
- Static progressive
- Serial static
But how do you decide which type to use? In this blog post, we offer an evidence-based assessment to help you in this decision-making process. But first, let’s review the different types of mobilization orthoses.
Types of mobilization orthoses
Dynamic
Dynamic orthoses typically incorporate elastic components and coils or springs. These put tension on a joint to increase passive range of motion.
Aside from that, dynamic mobilization orthoses can also be used to assist with weakened muscles or paralyzed nerves. They are often applied to aid in functional activities, such as with peripheral nerve injuries where muscles are weakened or paralyzed.

Functional Ulnar Nerve Orthosis in Orfit Colors NS – Sonic Silver.
The springs and/or coils can help substitute for the weak or paralyzed muscles, which is very helpful in cases of radial, ulnar, or median nerve palsy.
Dynamic mobilization orthoses can also be used with stiff joints that lack a full range of motion.
Static progressive
Static progressive orthoses incorporate non-elastic components. They apply force to a joint to hold it in its end range position to improve passive joint range of motion.
Examples of these static components are:
- Gears
- Monofilaments
- String or fishing lines
- Velcro® hook and loop tape
- Turnbuckles (devices which allow for regulation of tension)

Static progressive finger flexion cuff in Orficast 3 cm.
Static progressive orthoses allow progressive changes in joint position. This happens as the passive range of motion of the involved joint changes and improves over time.
Serial static
Serial static orthoses hold a stiff joint or tight shortened tissue in its end range position to increase passive range of motion or tissue length.
Every few days or even once a week, the therapist removes the orthosis and performs treatment to the stiff or contracted joint. Then they apply a new orthosis to the client in a new end range position.

Static progressive mobilization orthosis in Orficast 3 cm.
Serial static orthoses are very useful in the treatment of stiff joints:
- PIP joint flexion contracture
- Extrinsic wrist tightness following fractures/trauma
- First web space tightness following trauma/fractures
So, which one do you choose?
Depending on the patient and the specific injured joint, the therapist can decide on one of these orthoses. All three of them help to regain tissue length and improve joint range of motion.
For example, a dynamic orthosis might be the solution for patients with nerve palsy (e.g. radial nerve palsy) and/or weakened muscles, because these types of orthoses can allow for functional motion.
Selecting the most appropriate mobilization orthosis for your client is an important decision. It should be based on sound clinical reasoning and supporting evidence.
Evidence-based assessment
The following information can help you decide on an appropriate orthosis for your patient.
Soft End Feel vs. Hard End Feel
When assessing a patient with a stiff joint and/or limited joint range of motion, you can subjectively determine whether the specific joint has a soft end feel or a hard end feel.
End feel is the type of resistance felt when passively moving a joint through the end range of motion. You can evaluate the type of end feel by applying pressure to the joint at the end of the available passive range:

Soft end feel
The soft tissues give way with a small amount of pressure
The soft end feel can be described as a joint with immature scar tissue in the joint structures. You can choose any type of mobilization orthosis to address the limitations in motion.
Hard end feel
You need firm pressure to mobilize the joint further than the limitation.
The hard end feel can be described as a joint with mature scar tissue. It might respond best to serial static or static progressive orthoses.
The Modified Weeks Test
The Modified Weeks Test is an assessment that you can do before orthotic fabrication. It helps to clarify what type of mobilization orthosis may be most appropriate for your patient.
The test follows a few steps:
- First, the therapist performs a “cold reading” of the stiff joint’s passive range of motion.
- Then, the patient places their hand in a heated modality such as a fluido-therapy unit or a heated whirlpool. In this way, the stiff joint can be mobilized for 20 minutes.
- The therapist places the stiff joint in its end range position. This involves a tolerable over-stretch and heat application for another 10 minutes.
- After the 30 minutes of heat and mobilization, the therapist takes a “preconditioned reading” to measure the passive range of motion.
- Finally, the therapist compares the “preconditioned reading” to the “cold reading”.
The difference between the two passive joint range of motions (preconditioned and cold reading) can influence the orthotic selection:
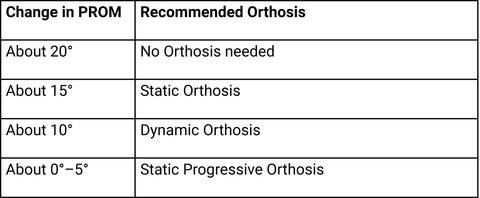
The Modified Weeks Test helps you choose the most suitable mobilization orthosis.
The author Ken Flowers proposed this decision making assessment in 2002, but stated that he had little evidence to support it. However, Glasgow et al. also used this assessment in their study on dynamic orthoses for stiff finger joints in 2011. They found it to be an accurate and reliable measure.
In conclusion
Using an evidence-based method can assist you in your clinical decision making. You can apply it the next time you have a patient with a stiff joint and you are considering an orthosis to help regain passive motion.
The possibilities are endless when it comes to dynamic splinting. Have a look at our Dynamic Splinting Guides for inspiration.
References
> Schultz-Johnson, K. (2002). Static progressive splinting. Journal of Hand Therapy, 15(2), 163-178.
Written by Debby Schwartz, OTD, OTR/L, CHT
Physical Rehabilitation Product and Educational Specialist at Orfit Industries America.
Debby is a hand therapist with over 34 years of clinical experience. She completed her Doctorate of Occupational Therapy at Rocky Mountain University of Health Professions in 2010.
She is also an adjunct professor at the Occupational Therapy Department of Touro College in NYC and has written many articles for hand therapy journals, including the ASHT Times and the Journal of Hand Therapy.
